May 3, 2016
On April 27, 2016, the Centers for Medicare & Medicaid Services (“CMS”) released the highly anticipated proposed rule that would implement major provisions of the Medicare Access and CHIP Reauthorization Act of 2015 (“MACRA”) affecting physician payment under the Medicare program (“Proposed Rule”). The Proposed Rule sets forth an approach to structuring and paying physicians under two “tracks” in the new Quality Payment Program—the Merit-Based Incentive Payment System (“MIPS”) and advanced alternative payment models (“Advanced APMs”). CMS will consider stakeholder comments submitted through June 27, 2016 and will issue a final rule prior to the start of the 2017 calendar year performance period.
The MACRA established two tracks for reimbursing physicians under the Medicare physician fee schedule starting in 2019—the MIPS and Advanced APMs. The MIPS combines the existing Physician Quality Reporting System (“PQRS”), Value Modifier (“VM”), and Meaningful Use programs, along with a new measure category for Clinical Practice Improvement Activities (“CPIAs”), into a single performance measurement and payment adjustment program. CMS expects most providers will report measures and be subject to payment adjustments under the MIPS, as it represents the default payment mechanism for physicians not participating in Advanced APMs.
The Advanced APM track would exempt qualifying APM professionals (“QPs”) and partial qualifying APM professionals (“Partial QPs”) that satisfy thresholds for revenue or patient lives under Advanced APMs from MIPS reporting and payment adjustments. The MACRA contained significant incentives to encourage clinicians to participate in Advanced APMs, including a 5% bonus from 2019 through 2024 on a clinician’s total professional Medicare claims for the prior year. As we detail further below, the CMS set a high bar for payment models that satisfy the Advanced APM criteria. Indeed, 95% of the ACOs currently participating in the Medicare Shared Savings Program (“MSSP”) would not qualify as an Advanced APM under CMS’s proposed criteria. This is a significant development and will have downstream implications for providers’ transition to more challenging APMs that involve downside risk.
Merit-Based Incentive Payment System
As noted above, a majority of physicians are likely to remain in the MIPS. MIPS eligible clinicians would include all physicians, nurse practitioners, physician assistants, clinical nurse specialists, registered certified nurse anesthetists, and groups including such professionals who are not QPs, Partial QPs, or subject to one of the very narrow exclusions. Measurement across the performance categories would occur at both the individual (NPI) and group (TIN) level. CMS has proposed using the full 2017 calendar year as the performance year on which 2019 payment adjustments will be based.
In general, the measures to be used in the MIPS resemble those used in the PQRS, VM, and Meaningful Use programs. However, CMS has proposed significant changes to how performance will be scored and has provided clinicians greater flexibility in choosing the measures under which they will be evaluated. Below is a brief explanation of how clinicians will be measured under each performance category:
Quality. Eligible clinicians or groups would report at least six quality measures, including a cross-cutting measure and at least one outcome measure or other high priority measure. Clinicians and groups would be permitted to select the measures against which they will be evaluated from a list of all MIPS measures or a set of specialty-specific measures (which may include fewer than 6 measures). CMS proposed different standards for non-patient-facing clinicians because of the relative dearth in specialty-specific measures for some specialties.
Resource Use. This measure would be calculated for attributed Medicare beneficiaries using the (1) total per-capita cost for all attributed beneficiaries measure; (2) the Medicare spend per beneficiary measure; and (3) newly proposed condition and episode-based measures. CMS will adjust data to reflect differences in geographic payment rates, beneficiary risk factors, and physician specialties. CMS would evaluate performance at the individual (TIN/NPI) and group (TIN) levels using attribution logic similar to that found in the VM program.
CPIA. This is a new measure category for the MIPS that would encourage physicians to adopt clinical delivery models and capabilities that are consistent with CMS’s Triple Aim goals. To achieve the highest potential score, clinicians or groups would choose 3 high-weighted CPIAs (20 points each), 6 medium-weighted CPIAs (10 points each), or any other CPIA combination to achieve a total of 60 points. Clinicians and groups participating in APMs would automatically receive 30 points (50% of CPIA total), and those in patient-centered medical homes automatically receive the full 60 points (100% of CPIA total). Other CPIA measure subcategories relate to expanded practice access, population management, care coordination, beneficiary engagement, patient safety and practice assessment, achieving health equity, emergency response and preparedness, and integrated behavioral and mental health.
Advancing Care Information. This measure category would replace the Meaningful Use program and would align the performance period with the other measure categories. Clinicians that report measures under the quality performance category using certified EHR technology would be treated as having satisfied the CQM reporting requirement under current law. Performance would be assessed and aggregated at the group level as if it would have been submitted individually. Half of the score would be based on reporting numerator and denominator figures for measures in Stage 3 of the Meaningful Use program. The remaining 50% is based on clinicians’ performance on 8 measures. A bonus point would be awarded for reporting to public health and clinical data registries. The scoring method on the performance portion provides multiple routes for clinicians to achieve greater than a 100% total score, which helps alleviate concerns that practices with less advanced capabilities will be penalized, and that scoring will be “all or nothing.”
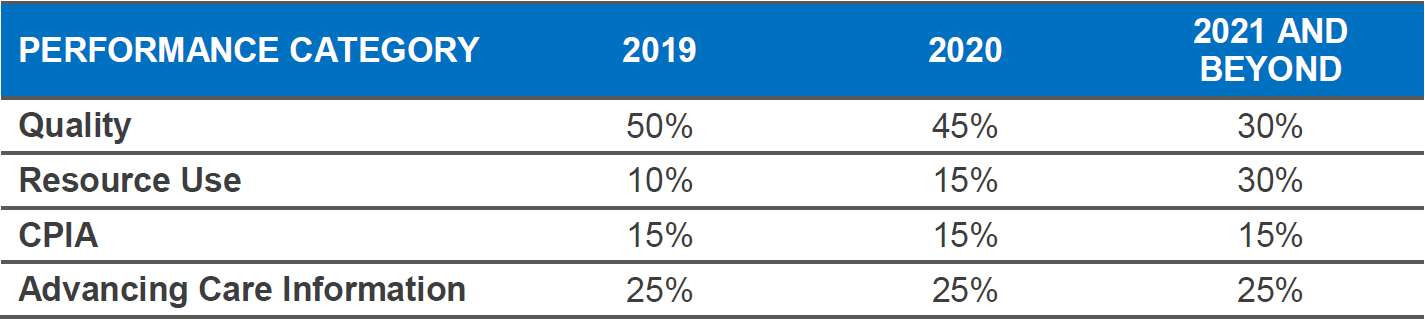
The weighting for MIPS performance categories that would be used to determine the composite performance score and the MIPS payment adjustment are as follows:
CMS also proposed a reporting and scoring mechanism for eligible clinicians participating in so-called MIPS APMs (not to be confused with Advanced APMs) that have separate reporting requirements for quality and cost/efficiency. For qualifying MIPS APMs, CMS will permit APM entity groups (i.e., all clinicians on the APM participant list) to aggregate clinician performance data on APM measures to satisfy their reporting obligation under the MIPS. CMS will evaluate the aggregated data and assign a MIPS composite score and corresponding payment adjustment to all clinicians in the APM entity group (i.e., all clinicians on the APM participant list). CMS will retain the authority to reweight MIPS scores to reflect the differences between the standard MIPS measure sets and the measures reported through each APM. This approach should minimize administrative burden and any conflicts that might otherwise result from the overlap between reporting measures under both the MIPS and various APMs.
Advanced Alternative Payment Models
The Proposed Rule sets forth the minimum criteria for an Advanced APM, which must be satisfied for eligible clinicians to be exempt from MIPS and eligible to receive the 5% incentive payment starting in 2019. To the disappointment of many in the provider community, CMS did not include many popular APMs in its definition of Advanced APMs. Under the proposed criteria, MSSP Track 1 ACOs, the Bundled Payments for Care Improvement Initiative, and the Comprehensive Care for Joint Replacement Model, among others, would not qualify as Advanced APMs. MSSP Track 2 and Track 3 ACOs, the Next-Generation ACO Model, and the recently announced Comprehensive Primary Care Plus (CPC+) model, would qualify as Advanced APMs.
CMS proposed requiring Advanced APMs to strictly satisfy the rigorous qualification requirements in the MACRA, including that: (1) the APM must require participants to use certified EHR technology; (2) the APM must provide for payment for covered professional services based on quality measures comparable to those in the quality performance category under the MIPS; and (3) the APM must either require that participating APM entities bear risk for monetary losses of more than a nominal amount under the APM, or be a medical home model expanded under CMMI’s Section 1115A authority.
CMS proposed a higher standard for financial risk bearing than many in the provider community had hoped. Advanced APMs must include provisions that, if actual expenditures for which the APM entity is responsible under the APM exceed expected expenditures during the performance period, CMS may: (1) withhold payment for services and/or the APM entity’s eligible clinicians; (2) reduce payment rates to the APM entity and/or its eligible clinicians; or (3) require the APM entity to owe payments to CMS. While CMS acknowledged the significant investments that many MSSP ACOs have made to develop population health management capabilities and infrastructure, CMS did not believe that sort of business risk satisfied the statutory requirement in the MACRA. Consequently, only those ACOs that share financial risk under the proposed nominal amount standard (based on marginal risk, minimum loss rate, and total potential risk thresholds) will qualify as Advanced APMs.
As noted above, QPs and Partial QPs that satisfy the minimum requirements for participation in an Advanced APM will be eligible for a 5% bonus from 2019 through 2024 based on the clinician’s total previous year’s Part B professional claims. In addition to satisfying CMS’s Advanced APM criteria, QPs and Partial QPs must have a sufficient percentage of their Medicare revenue (and all-payer revenue in later years) flowing through Advanced APMs. CMS also proposed a method that considers the number of attributed Medicare patients in the Advanced APM (and all-payer patients in later years). For 2019, QPs must receive 25% of their Medicare payments through the Advanced APM or have 20% of their patients attributed through an Advanced APM. For 2019, Partial QPs must receive 20% of their Medicare payments through the Advanced APM or have 10% of their patients attributed through an Advanced APM. Partial QPs would have the option to report measures under the MIPS and be subject to a positive, negative, or neutral payment adjustment; however, they would not be eligible for the 5% incentive payment or the APM conversion factor that takes effect for 2026. The revenue and patient count thresholds for Advanced APMs increase over time and begin to consider all-payer revenue and patient counts in 2021.
CMS proposed to classify eligible clinicians for each APM entity based on the participant list as of December 31st of each QP performance period. CMS further proposed to make QP determinations at a group level. As a result, QP determinations for the group would apply to all the individual eligible clinicians who are identified as part of an Advanced APM entity (e.g., all eligible clinicians participating in a qualifying ACO). If that eligible clinician group’s collective threshold score meets the relevant QP threshold, all eligible clinicians in that group would receive the same QP determination for the year. Calculations used to arrive at the QP determination are aggregated using data for all eligible clinicians participating in the Advanced APM entity during the performance period. The performance period is the full calendar year that aligns with the MIPS performance period.
Conclusion
The Proposed Rule reflects a commitment by CMS to address the many shortcomings in the current Medicare physician payment system. Although likely to be subjected to ongoing scrutiny from the provider community, the proposed changes to the reporting and scoring structure in MIPS aim to reduce administrative burden and complexity and increase flexibility and transparency. While it is too early to tell how MIPS will ultimately impact providers, the provisions in the Proposed Rule, if implemented, would significantly improve the manner in which clinicians are evaluated by Medicare.
With respect to Advanced APMs, CMS has continued its aggressive effort to transition providers to more aggressive APMs that involve two-sided risk. Coupled with the new Track 3 ACO, the Next-Generation ACO Model, and the payment waivers and enhanced beneficiary engagement tools reserved for these advanced models, the Proposed Rule exemplifies CMS’s belief that success in achieving the Triple Aim requires providers to transition to two-sided risk. Those providers that are willing to make the transition for the 2017 performance year have an opportunity to gain significant advantages under the new Quality Payment Program.
If your organization needs help plotting its APM strategy, if you have questions relating to the provisions of the Proposed Rule, or if you would like Hancock Daniel’s assistance in preparing and submitting formal comments before the June 27, 2016 deadline, please contact Jim Daniel.
Authored by:
The information contained in this advisory is for general educational purposes only. It is presented with the understanding that neither the author nor Hancock, Daniel & Johnson, P.C., PC, is offering any legal or other professional services. Since the law in many areas is complex and can change rapidly, this information may not apply to a given factual situation and can become outdated. Individuals desiring legal advice should consult legal counsel for up-to-date and fact-specific advice. Under no circumstances will the author or Hancock, Daniel & Johnson, P.C., PC be liable for any direct, indirect, or consequential damages resulting from the use of this material.


